Effective 5/1/2019, BCBS IL made some changes regarding their Medicare Supplement Products. The plans are staying the same and are guaranteed to issue, but there are some changes in:
-
New rate determiners (gender and tobacco use)
-
New rates
-
New paper application
-
The BCBS IL Plan Change Form will not be accepted
-
Changes in the online submission process via Retail Shopping Cart
-
Household Discounts (3% off premium)
-
Billing changes
-
New membership system
-
Producer access to member communications
-
Missing Information Process
-
Some applicant information will not be available in the Retail Producer Portal
-
Commission clarification with changes
-
New contact information for support of the new plans
New Rate Determiners
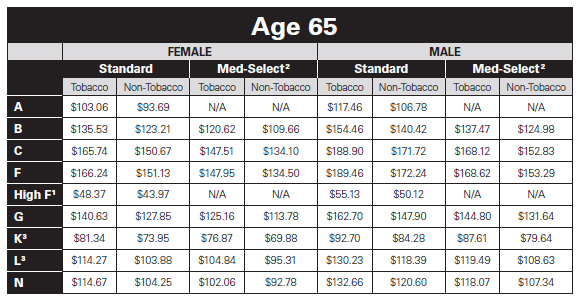
Gender and tobacco use now affect rates. It appears that women’s rates are lower while men’s rates are higher and tobacco use for either gender will increase rates as well. The new rate charts will look like this:
Plans sold with an effective date prior to 5.1.19 will continue and these plans are called legacy plans. When selling plans with an effective date of 5.1.19 and after, be sure to use the correct application.
New Paper Application
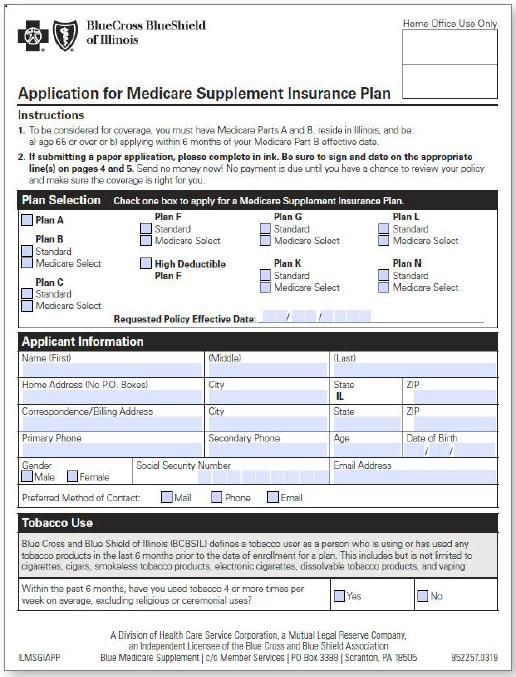
BCBS IL will no longer accept the Plan Change Form as of 5/1/2019. If a client decides to move from their legacy plan to a new plan, they would need to complete the new application and answer the rate determiner questions.
Applying Online Via Retail Shopping Cart
BCBS strongly recommends enrolling online versus submitting “paper” or pdf applications. There are fewer errors and shorter turnaround times with online applications.
Starting in May, you will see the following changes to the Retail Shopping Cart:
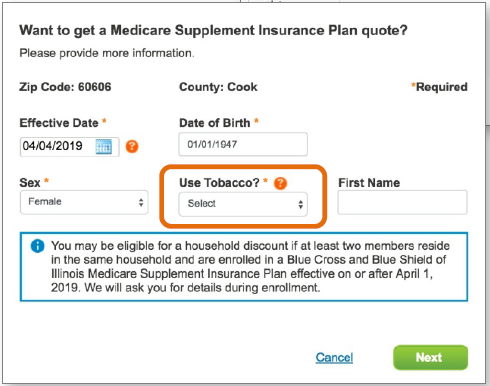
On the “census” screen, “Use Tobacco?” will be included and must be answered to move to the next step.
Users can click on the question mark next to “Use Tobacco?” to get more information about what qualifies as tobacco use.
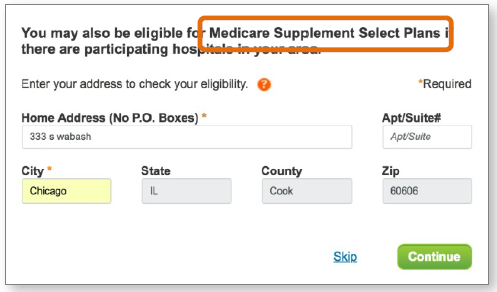
Your client may be eligible for Medicare Supplement Select Plans. Entering the entire physical address determines if the user is eligible.
The user must live within a certain distance from Select Plan providers to qualify. If the address provided is Select Plan eligible, the user will see a confirmation at the top of the screen.
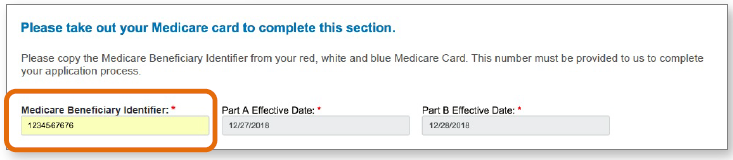
After selecting a plan, the enrollment process begins. Note that the Medicare Beneficiary Identifier number is required.
Household Discount
Applicants have the option of applying for the Household Discount. The user should submit the qualifying household member’s name and policy number. If the household members are applying at the same time, the policy number is not required.
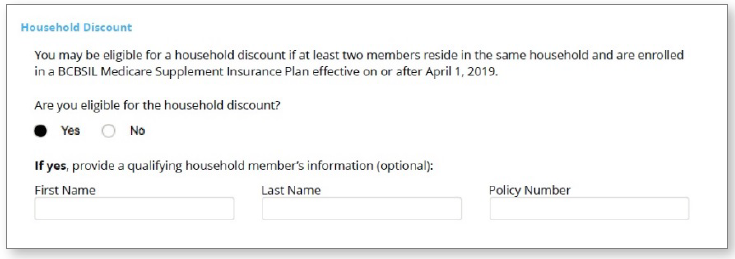
- Discount is only available for members applying for one of the new Medicare Supplement plans, not the legacy plans
- The discount is 3% of the monthly premium. The discount will appear in the bill/invoice
- To qualify, the member must live with a member who is also enrolled (or applying at the same time) in one of the new plans
- If the applicant qualifies, the discount is applied post rating after validation
- If the applicant receives the discount and leaves the household, the discount still applies
- Producer compensation is based on premium after the discount is applied
Billing and Payments
Reminder: Applicants may select a billing date from the 1st through the 28th of the month.
Applicants of new plans can choose their billing frequency:
- Monthly
- Quarterly
- Semi-annual
- Annual
- Note that bi-monthly billing will not be available to members of new Medicare Supplement plans with effective dates of May 1 or later.
Members of new plans can choose from the following payment channels to submit their premiums:
- Automated electronic withdrawal Click here for the EFT form
- Check by phone (see contact numbers and hours of operation at the end of the blog)
- Payment through the member’s bank
- Mail-in check (members should use the mailing address on their invoices)
Billing Delinquencies
- If a legacy plan is canceled due to billing delinquency, the member can reinstate the same plan as long as the full premium payment needed is received within 60 days of the termination date, which also means no gap in coverage.
- If the legacy plan is canceled due to non-payment of premium, and the member is within the 60 day reinstatement period, but does not want to pay the premium needed to reinstate the legacy policy, the member will need to re-enroll in a new Medicare Supplement plan. In this case, there will be a gap in coverage, and the legacy plan will not be available.
- Payments received 61 or more days from the policy cancelation date will be refunded.
New Membership System
- In a continuous effort to streamline processes and better serve our customers, members enrolling in new Medicare Supplement plans will be placed in a new membership platform.
- Members with legacy Medicare Supplement plans will remain on the current membership system. In the future, we will move these legacy members to the new membership system.
- Depending on your client’s plan (legacy or new), they will have slightly different enrollment and service experiences. Communications, payment options and application processing will be different.
Producer Access to Member Communications
- BCBS will no longer mail physical copies of member letters to the producer of record.
- As BCBS focuses on moving new Medicare Supplement members to the new membership platform, digital copies of member correspondence are not yet available via the Retail Producer Portal. They are working to provide producers with digital copies of member correspondence via the portal. Producers with clients enrolled in legacy plans will continue to see those members’ correspondence in the portal as they do today.
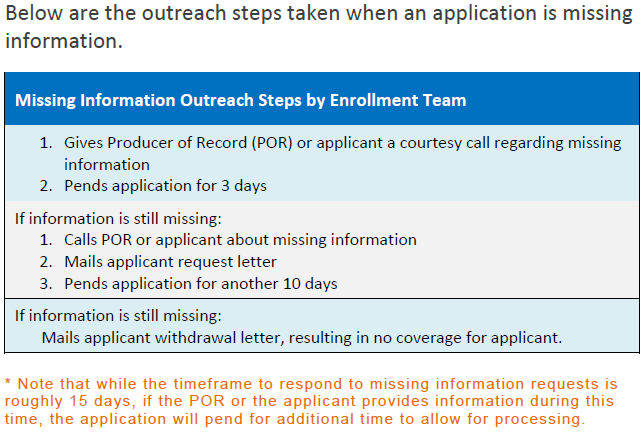
Request for Missing Information Process
Applications go into a pending status when the application is not properly completed or the wrong application is submitted.
Member Materials
Once the enrollment application is processed, BCBS will mail fulfillment kits and ID cards to the new member within 10 business days of enrollment approval.
Fulfillment kits and ID cards are sent separately, via priority mail.
Members enrolled in Legacy Plans choosing new plans
Members enrolling in a new plan will receive a New Member ID Card and Number. The ID card and number from the legacy Medicare Supplement plan will be deactivated.
Members who transition from a legacy plan to a new plan will receive a new member fulfillment package.
If you use the Retail Producer Portal or Blue Access for Producers to track your clients, you will have two different client files for the same member, one with the legacy plan ID and one with the new plan ID for a period of time. In addition, agent commission statements will reflect both member accounts for the same client.
Our enrollment specialists will try to keep the same premium billing due date for members who transition from a legacy plan to a new plan.
For applicants of new plans, some correspondence, payment and application data will be unavailable in the Retail Producer Portal:
- PDF of the completed app
- The “Decision” display
- The app withdrawal date
- Email address and cell phone number (once the applicant becomes a member, all contact information will be available)
- If there’s a rate change, the reason won’t display but the rate amount will display
Legacy plans will continue to have the same information in the Retail Producer Portal as they did previously.
Medicare Supplement Commissions
There are no changes to the Medicare supplement commission rates.
Re-enrollments & Reinstatements
- The producer is paid according to the original effective date as detailed in the Medicare Supplement commission schedule.
- Reinstatements, re-enrollments, plan changes and replacements (with or without a gap in coverage) are not considered new or first year sales.
- Reminder: A replacement policy is considered a renewal for commission purposes. Replacements include moving from a legacy plan to a new plan or moving from a plan with another insurer to a BCBSIL plan.
Household Discounts
- Consumers can apply for a household discount (a 3% discount off the premium) when enrolling in new Medicare Supplement plans.
- The household discount is not available with legacy plans.
- Compensation for Medicare Supplement policies is based on the premium.
- If members qualify for the household discount, compensation will be paid on the new discounted premium. Commission adjustments will occur the month subsequent to the change.
Contacts
| Producer Support Product information • Sales Assistance • Application Status • Policy Changes • Retail Producer Portal | Phone: 877-587-6638 Fax: 855-867-6714 8:00 a.m. to 5:00 p.m. CT, Monday through Friday |
| Producer Service Center Commissions • Producer of Record Changes • Book of Business Inquiries • Licensing | Phone: 855-782-4272 Email: Producer_Service_Center@hcsc.net 8:00 a.m. to 5:00 p.m. CT, Monday through Friday |
| Member/Customer Service Enrollment • Benefits • Claims • Appeals • Preauthorizations | Phone: 877-384-9297 Fax: 855-867-6717 7:00 a.m. to 6:00 p.m. CT, Monday through Friday |
| Member Check-by-Phone* Make a One-off Bank Account Premium Payment | Phone: 800-611-1767 IVR System available 24 hours a day, 7 days a week* |




Leave A Comment
You must be logged in to post a comment.